Dec 02 2025
/
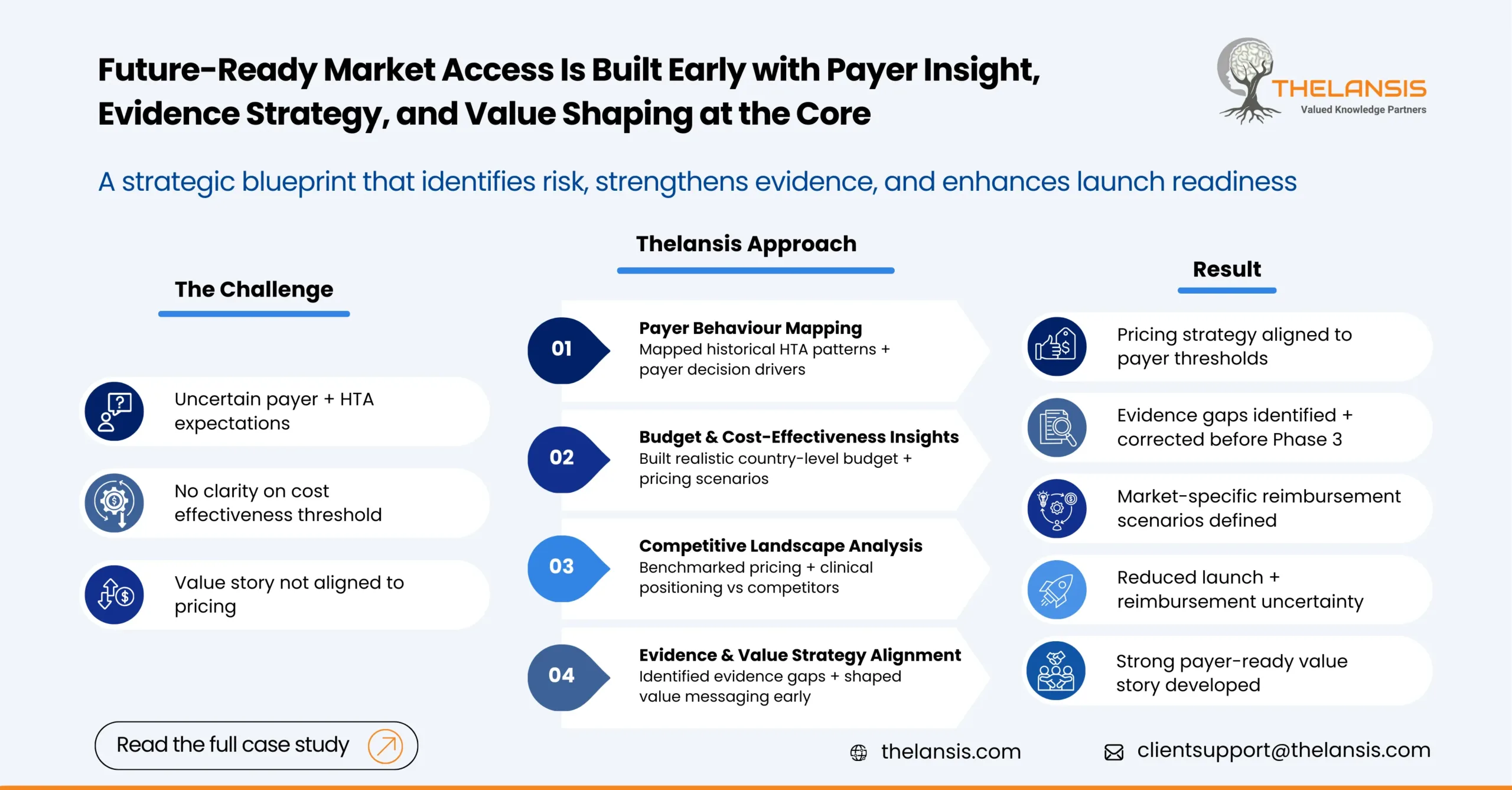
Strengthening Global Market Access Readiness Through Early Payer & HTA Planning
Introduction:
A global biopharma company preparing to advance towards asset commercialisation approached Thelansis with a clear priority that they wanted to enter multiple markets with confidence that their clinical evidence, pricing expectations, and value communication would withstand payer scrutiny. The therapy showed strong early promise, but the success in Phase 3 does not automatically translate into smooth reimbursement pathways, especially in regions where HTA bodies demand tight alignment between clinical value, real-world relevance, and economic justification.
Over the past decade, Thelansis has supported companies in similar transitions by helping them understand how payers think, what evidence resonates, and where access bottlenecks typically arise.
Problem Statement:
The client faced three immediate challenges:
- Uncertainty around payer expectations across the U.S., EU5, Japan, and selected emerging markets, particularly in unmet need, differentiation, and acceptable price ranges.
- Lack of clarity on cost effectiveness thresholds and budget impact constraints that could shape HTA recommendations and market access timelines.
- No unified value story linking clinical outcomes to economic arguments across diverse healthcare systems.
Without early insights into payer behaviour and competitive dynamics, the risk of delayed reimbursement, price erosion, or restricted access was significant.
Objective:
The primary goal was to build a forward-looking market access roadmap that helped the client:
- Anticipate payer and HTA reactions well before launch
- Identify evidence gaps that could weaken the value proposition
- Develop pricing scenarios tied to real budget realities
- Prepare internal teams for the reimbursement hurdles in major markets
Thelansis proposed a structured assessment integrating payer insights, health-economic expectations, and competitive context to guide clinical, commercial, and HEOR planning.
Methodology:
Our team applied a multi-layered evaluation centred around how payers make decisions rather than simply summarising policy documents.
A) Payer Behaviour & Decision Drivers
We analysed historical reimbursement patterns for comparable therapies, including how HTA bodies reacted to similar endpoints, comparators, and safety profiles. This included:
- Review of past coverage decisions and appraisal dossiers
- Mapping of payer priorities (clinical relevance, unmet need, cost offsets, equity considerations)
- Assessment of real-world evidence requirements across markets
B) Budget Impact & Cost-Effectiveness Thresholds
We reviewed local disease burden, treatment patterns, and expected adoption to understand how each health system would absorb the new therapy
- Built country-level budget impact estimates to clarify potential payer pressure
- Evaluated how the asset aligns with typical cost-effectiveness ranges applied by HTA bodies in different regions
- Tested pricing and access scenarios to reflect the realities of payer negotiations
C) Competitor Pricing & Landscape Pressure
We evaluated how the asset would be judged relative to current and upcoming competitors
- Pricing benchmarks and negotiated discounts
- Treatment sequencing trends across markets
- Expected payer pushbacks based on comparative performance
D) Evidence & Value Strategy Mapping
We highlighted where evidence was strong, where it might be challenged, and what would be needed to secure favourable recommendations.
- Priority HEOR analyses to initiate
- Real-world evidence opportunities
- Clinical endpoints most likely to resonate with payers
- Narrative framing for global and local value dossiers
Result:
The engagement delivered a clear, actionable picture of the market access environment long before the client reached the submission stage.
Key outcomes included:
- A refined pricing strategy anchored in real payer thresholds, not internal assumptions
- Early identification of evidence gaps, allowing the clinical team to adjust protocol elements and collect supportive real-world data
- Market-by-market access scenarios, outlining best-case, base-case, and risk-case reimbursement timelines
- A sharper, evidence anchored value story tailored for HTA bodies and payer discussions
- Reduction in launch uncertainty, as internal teams now understood the trade-offs shaping access decisions
The client used this work to guide its global launch preparation, align their cross-functional teams, and prioritize markets with the highest likelihood of early access. The insights also influenced their Phase 3 planning, ultimately strengthening their negotiation position across multiple regions.

